Funded by The Brain Tumour Charity, this research aims to pioneer the diagnosis of medulloblastoma by using minimally invasive methods, protecting the quality of life of children with this diagnosis.
Medulloblastoma is the most common cancerous childhood brain tumours, accounting for 15-20% of all childhood brain tumour diagnoses. Around 52 children are diagnosed with a medulloblastoma each year in the UK.
These tumours are fast growing and develop at the back of the brain in the cerebellum.
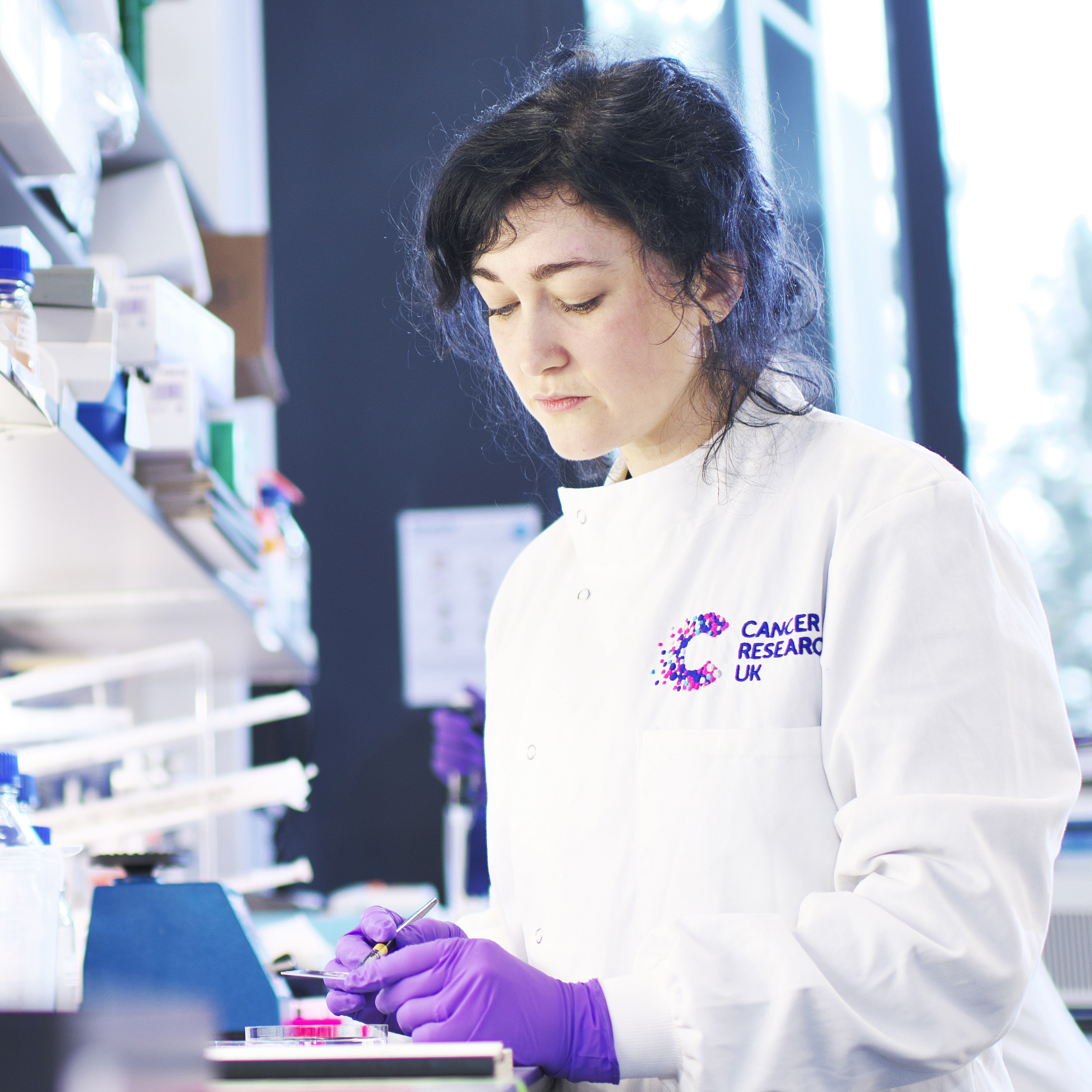
Dr Jessica Taylor, a postdoctoral researcher at the University of Cambridge working in Professor Richard Gilbertson’s lab at the Cancer Research UK Cambridge Institute, will focus on one of the four subtypes of medulloblastoma - wingless (WNT) medulloblastoma. WNT-medulloblastoma is typically difficult to operate on, but is highly curable with chemotherapy and radiation.
The Brain Tumour Charity’s Future Leaders Award will enable Dr Taylor to explore a novel method to identify WNT medulloblastoma without using invasive surgery. This will protect children from the potential long-term, damaging effects of surgery such as memory problems and speech issues.
The research will use antibodies which are designed to bind to the WNT-medulloblastoma cells. Once bound to the cells, they will be visible on a PET scan and can be used to diagnose this subtype of medulloblastoma.
Researchers will also design these antibodies to bind to drugs that could treat WNT-medulloblastoma. This innovative approach would deliver treatments directly to the tumour, potentially replacing the need for more traditional chemotherapy. This could have several benefits including giving patients an additional treatment option and offering a more targeted therapy, potentially reducing the side effects from treatment.
John Huggins’ granddaughter Sophie Harper was diagnosed with medulloblastoma in 2006.
John said: “Until the age of nineteen months Sophie seemed to be a normally developing little girl, she walked at eleven months and her speech was well ahead of her age. From nineteen months she started to vomit regularly and when her mother took her to the doctors on day four, he diagnosed a virus. After ten days my daughter returned to the doctor, but again he said it was a virus. Sophie was taken to the doctor a number of times over the next two and a half months and there was no change with the doctor’s diagnosis. Sophie then started to lose her ability to walk, no longer was she the happy child she was, complaining of head pain, started falling over regularly and wanting to be carried around. It was only then the doctor agreed for Sophie to have a scan.”
Sophie’s scan took place at Norwich University Hospital and revealed a mass on her cerebellum. She was transferred to Addenbrooke’s Hospital, Cambridge, for further tests and a medulloblastoma tumour was confirmed.
John said: “None of us had any knowledge of brain tumours and it became a huge learning curve. At that point Mum and Dad had to decide whether to take the option of curative or palliative care. Sophie always had a big personality and was such a fighter with any illness, so Mum and Dad decided they had to give her the tools to fight with and take the curative option”.
The following week, Sophie underwent an operation to try and remove the tumour and the family waited anxiously in the garden of Addenbrooke’s Hospital for news. The operation was expected to last around three to four hours but Sophie was in surgery for seven and a half.
John said: “Sophie didn’t regain consciousness for thirty two days, due to the insult to her brain. She spent three months in intensive care and was now needing an oxygen supplement and having to be fed through a gastrostomy tube. Both of these would stay for the next six years of her life.
“It also became clear that there were other side effects from the operation: her speech was significantly impacted and she was unable to hold our gaze and her movements were uncoordinated and clumsy. During the time of her treatment she received more than a hundred transfusions of blood products due to low blood cell counts, but none of us can remember a single day, when she didn’t make us laugh or brighten our day. She had an amazing ability to do that.
“It is true to say, surgery had a dramatic effect on Sophie, she was no longer the child we knew before the operation.”
Just before Sophie’s eighth birthday, her family were devastated when a scan revealed another growth on her brain. She was given three months to live, but survived almost a year and sadly died shortly before her ninth birthday in 2013.
After her death, Sophie’s family set up The Sophie Elin Harper Fund with The Brain Tumour Charity to raise funds and awareness of brain tumours. Their fundraising to date totals a remarkable £38,000.
John said: “The side effects Sophie had following surgery, with the insult to her brain, were huge and totally life changing.
“Sophie lived a very cruel life, in and out of hospital. Even the shunt fitted in her brain had to be replaced on three occasions. She never regained the ability to walk, and was always fed through a gastrostomy tube, together with an oxygen supplement, but she never complained.
“The possibility of avoiding side effects and unnecessary surgery would be a real turning point in the treatment of medulloblastoma.”
Dr Jessica Taylor, The Brain Tumour Charity Future Leader at the University of Cambridge said: “Over 50 children in the UK are diagnosed with medulloblastoma every year and ensuring that these children get the best treatment is of paramount importance to ensure they have a good quality of life.
“We know that WNT- medulloblastoma is difficult to resect surgically, but responds well to standard of care treatment. We hope that our research can avoid unnecessary surgeries in the future.
“With 1 in 4 children with this tumour type suffering long-term memory loss and speech issues after surgery, it is important that we work towards improving diagnostic methods which avoid surgery.
Dr David Jenkinson, Chief Scientific Officer at The Brain Tumour Charity, which helped fund the project, said: “Our Future Leaders are the next generation of brain tumour researchers. Their innovative ideas and determination to find a cure will drive us closer to improving the lives of those diagnosed with a brain tumour. We are proud to be able to fund these brilliant minds.
“This innovative project exploits the features of WNT-medulloblastoma to create specific antibodies that will help diagnose and even treat this type of tumour, avoiding unnecessary surgery for the children diagnosed. Focussing research on non-invasive diagnostics and treatments help to prevent long-term damage that can result from surgery.
“This work will help deliver The Brain Tumour Charity’s aim of halving the harm that brain tumours cause.
“We very much look forward to following and sharing the success of this project in the future.”