Surgeons could soon eavesdrop on a patient’s brain activity during surgery to remove their brain tumour, helping improve the accuracy of the operation and reduce the risk of impairing brain function. BBC Look East's Science Correspondent, Richard Westcott finds out more...
Patients with low-grade gliomas in their brains – a slow-spreading, but potentially life-threatening tumour – will usually receive surgery to have the tumour removed. But removing brain tissue can be risky as there is no boundary between the brain and tumour – the tumour infiltrates the brain. Removal of tumour can lead to removal of vital parts of the brain and resulting impairments in functions such as speech, movement and executive function (which enables the individual to plan, organise and execute tasks).
To minimise this risk, neurosurgeons open the patient’s skull and then waken them. A local anaesthetic means the patient will feel no pain, and the brain itself contains no pain receptors.
The surgeon will probe the patient’s brain, applying mild electric pulses to tissue surrounding the tumour while asking them to perform a set of tasks. For example, the patient may be asked to count from one to five: if an electric pulse applied to a certain place in the brain affects their ability to perform this task, the surgeon will leave this tissue in place.
“As surgeons, we’re always trying to minimise the risk to patients and provide them with the best possible outcomes,” says Thomas Santarius, a neurosurgeon at Addenbrooke’s, Cambridge University Hospitals, and member of the CRUK Cambridge Centre Neuro-Oncology Programme.
“Operating on brain tumours is always a delicate balance between removing as much diseased tissue as possible to give patients better prognosis, while minimising the risk of damage to brain functions that will have a potentially massively detrimental impact on the patient’s life.”
While the current approach is considered the ‘gold standard’, it is not perfect. It takes time to apply the pulses on different parts of the brain and it may miss out some areas that are important for certain functions. The current battery of cognitive tests that surgeons use is also limited and does not test for the essential executive function, for example.
Now, a team of scientists and clinicians from the University of Cambridge and Addenbrooke's Hospital, led by Mr Santarius, Dr Yaara Erez and Mr Michael Hart, together with Pedro Coelho from Neurophys Ltd, has collaborated to develop a new approach that will enable patients to get a more accurate, personalised ‘read-out’ of their brain networks, and will provide surgeons with real-time feedback on the patient’s brain activity in theatre.
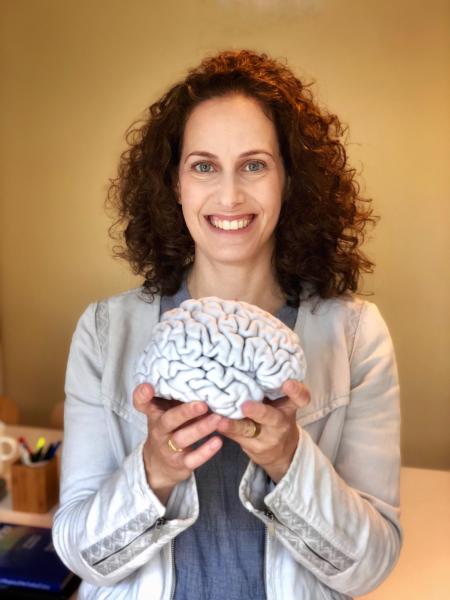
“At the moment, neurosurgeons only know about function in the average brain – they have no patient-specific information,” explains Dr Yaara Erez, a neuroscientist from the MRC Cognition and Brain Sciences Unit at the University of Cambridge. “But there’s been huge progress in brain imaging and electrophysiology – our understanding of the electricity within our bodies – so why not use this information to improve brain surgery? We are aiming to bring all this knowledge into the theatre, providing surgeons with integrated data and the best tools to support their work.”
Under this approach, patients would undergo a number of neuroimaging examinations using magnetic resonance imaging (MRI) before surgery aimed at identifying not only the exact location of the tumour but also how different regions of their brains communicate with each other.
As part of this process, a 3D-printed copy of the patient’s brain will be used, showing where the tumour is located. This model is intended to help surgeons plan the surgery, discuss with the patient the potential risks from surgery and involve the patient in decisions over which tissue to remove.
“Doctors need to be able to talk through the options with patients, and we hope that using neuroimaging data and presenting this as a 3D model will help surgeons with the planning of surgery and ensure patients are better informed about the risks and benefits from surgery,” says Dr Erez.
During surgery, once the patient’s skull has been opened, the surgeon will place electrodes on the surface of the brain, to ‘listen’ to their brain activity. A computer algorithm will analyse this information as the patient performs a battery of cognitive tests, giving live feedback to the surgeon. This will enable the surgeon to predict more accurately the likely impact of removing a particular area of brain tissue.
In particular, executive function is difficult to test using electrical stimulation – in part because it involves networks of regions across the brain. Dr Erez hopes that a combination of improved cognitive tests and a more accurate understanding of an individual patient’s networks will enable surgeons to monitor potential impairment to executive function during surgery.
“This isn’t going to replace brain stimulation during surgery,” says Dr Erez, “but it will guide the surgeon and it will save time and make surgery more efficient, more accurate. It will also enable us to understand how patients’ brains adapt to the presence of a tumour and how well they recover from surgery. It involves equipment that is largely already in use in surgeries, so should be easy and cost effective to implement.”
So far, the team has obtained data from 12 patients, already providing a large amount of data to analyse, with a rich dataset from each patient, collected before, during and after surgery. Although they are currently analysing this information offline, the data will help them find the best measures to provide the required information – what the ideal tasks for patients to perform are – and then to optimise the analysis.
The research has only been possible because of the interaction between researchers and clinicians from a variety of disciplines, says Dr Erez. “At Cambridge, we have different groups of neuroscientists with a range of expertise from psychology and imaging to computer science working with clinicians and surgeons at the hospital. Whatever we need, we can always find someone in Cambridge who knows how to do it!”
The research is supported by the Medical Research Council, the Royal Society and The Brain Tumour Charity.